As we did in 2025, The Imaging Wire asked key opinion leaders in medical imaging to provide their predictions on the technologies, clinical applications, and regulatory developments that will shape the specialty for the next 12 months. Here’s what they said…
3 Key Radiology Trends for 2026: Three fundamental trends will drive the radiology industry in 2026: 1) AI-based workflow will become more widespread and harder to differentiate. 2) Technology and services will increasingly be bundled to drive care-pathway product solutions. 3) Intense competition will continue, with partnering and M&A growing at a faster pace as healthcare spending tightens and price pressures get worse. Steve Holloway, CEO of Signify Research
AI Consolidation Shifts to Multi-Product Platforms: Radiology AI consolidation will continue and accelerate the shift from point solutions to multi-product platforms. A few vendors will emerge as market leaders, leveraging deeper workflow integration to deliver more value, offer broad bundles at lower prices, and scale adoption. Pure intermediary platforms will compete with vertically integrated players that have become platforms. OEMs will embed more AI through partnerships or acquisitions and enter the race. Finally, in a sustained AI bull market, more startups will reach nine-figure valuations. Amine Korchi, MD, radiologist and founder of Singularity Consulting
AI Vision Language Models Impact Radiology Reporting: Use of AI vision language models for draft report generation will be a major trend. Chest X-ray models are already seeing growing real-world evaluation – VLMs for modalities like CT and MRI are the next wave. Also watch for advancements in volumetric foundation models. Winning solutions will seamlessly streamline radiologist review-and-correction workflows. The real differentiator: multimodal fusion that integrates longitudinal clinical context with imaging. Woojin Kim, MD, CSO/CMIO at HOPPR and CMO at ACR Data Science Institute
Breast Density Loopholes to Close: Dense breast reporting is now a national standard, and many states have expanded insurance coverage for breast imaging. The federal Find It Early Act would close state-specific loopholes and include federal plans. The next challenge is educating women and providers about increased or high-risk factors and guiding appropriate supplemental screening and clinical choices. JoAnn Pushkin, executive director, DenseBreast-info
Breast Imaging Moves to Risk-Based Screening: Breast imaging will continue to move toward risk-based screening, optimizing screening intervals and modalities personalized to the individual, based on risk models that combine breast density, family history, genetics, and AI-derived imaging biomarkers. AI-enhanced risk stratification will continue to gain traction, using mammographic features such as density patterns, texture, and parenchymal complexity to refine a woman’s future cancer risk. This will allow women to be triaged into personalized screening pathways: high-risk patients directed to MRI/abbreviated MRI, or intermediate-risk women to modalities such as ultrasound and contrast-enhanced mammography. Stamatia Destounis, MD, managing partner, Elizabeth Wende Breast Care
CT Lung Cancer Screening Will Save More Lives: In 2026, CT lung cancer screening will save more lives than ever before. More countries will start screening programs (e.g., Germany), and more healthcare systems will achieve the “intersection of the curves”: More early-stage than late-stage lung cancer at diagnosis. Sebastian Schmidt, head of strategy, innovation, and medical affairs for CT at Siemens Healthineers
What Will Make MRI Safer? Last year the fatal Long Island MRI accident showed us just how tenuous our safety gains are. In 2026, more conversations should take place about which specific practices would make MRI safer, and how we go about making those standard across our profession, through regulation, licensure, or accreditation. Tobias Gilk, founder of Gilk Radiology Consultants
Opportunistic Screening Adds Value: 2026 will witness a rapid expansion of published studies demonstrating the added clinical value of AI-enabled opportunistic CT screening. Furthermore, the increasing clinical availability of these automated AI tools for cardiometabolic assessment should ultimately herald their routine use in value-added patient care. Perry Pickhardt, MD, chief of gastrointestinal imaging at the University of Wisconsin
Radiation Dose Management Tools: Practices will continue to become more comfortable using dose management tools to evaluate their dose data, benchmarking their doses for a given task against their peers. Diagnostic medical physicists play a crucial role in investigating and addressing dose outliers, and their important role in dose management will continue to grow. Cynthia McCollough, PhD, professor of medical physics and biomedical engineering at Mayo Clinic
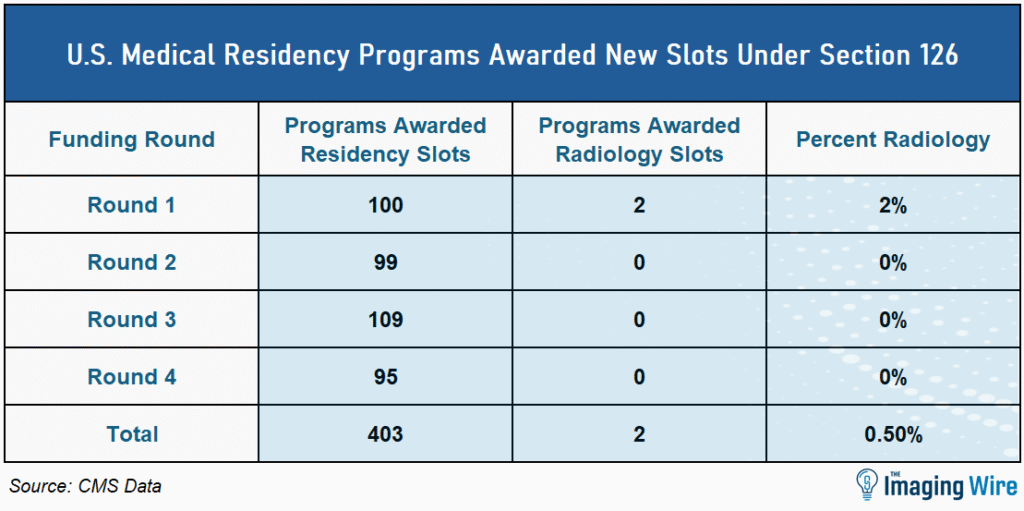
Radiologist Shortage Will Continue: Looking into 2026, the radiologist shortage remains acute. Imaging demand will continue to outpace training output, burnout will drive attrition, and AI won’t offset capacity gaps fast enough. Workforce pressure shifts from volume coverage to subspecialist scarcity, keeping recruitment and retention firmly center stage. Jay Gurney, director of radiology for Projectus
Regulation and Reimbursement: As hospital-based interventional procedures face their steepest revenue declines, groups with a strong IR background are recognizing the value of expanding into office-based labs as a necessary step to protect and diversify their revenue streams. Sandy Coffta, VP of client services at Healthcare Administrative Partners
Theranostics Emerges as Primary Treatment Option: Theranostics will continue to shed its reputation as a last-ditch treatment option, and dosimetry will become more routine. This upstream migration will be accelerated by emerging medium axial-field-of-view PET/CT scanners (~24-48 cm), which will increasingly deliver the sensitivity needed to reveal micrometastases missed by standard PET/CT systems, justifying earlier deployment of molecular therapies. Eliot Siegel, MD, professor, University of Maryland and co-founder of United Theranostics
The Takeaway
As healthcare’s most dynamic medical specialty, radiology is sure to continue its rapid pace of evolution in 2026. Rest assured that you can read about all the year’s top radiology trends in The Imaging Wire.