Smart MRI providers know patient comfort is linked to profitability. After all, the comfort quotient impacts image quality, diagnostic accuracy, operational efficiency, and patient satisfaction.
- Yet at least one-third of adult patients report distress, moderate anxiety, and discomfort related to MRI, according to a systematic review involving 220 patients.
When patients are claustrophobic or uncomfortable, it negatively impacts MRI providers…
- Fidgety patients lead to motion artifacts/poor quality images and the need to retake scans – impacting overall productivity.
- Sedating patients requires additional safety precautions, costing time and money.
- Cancellations and no-shows due to patient anxiety translate to lost revenue.
- Patients who have an uncomfortable MRI experience may go elsewhere next time – reducing repeat business and word-of-mouth referrals.
But it doesn’t have to be this way. Providers should seek out high-performance MRI systems designed with patient comfort in mind…
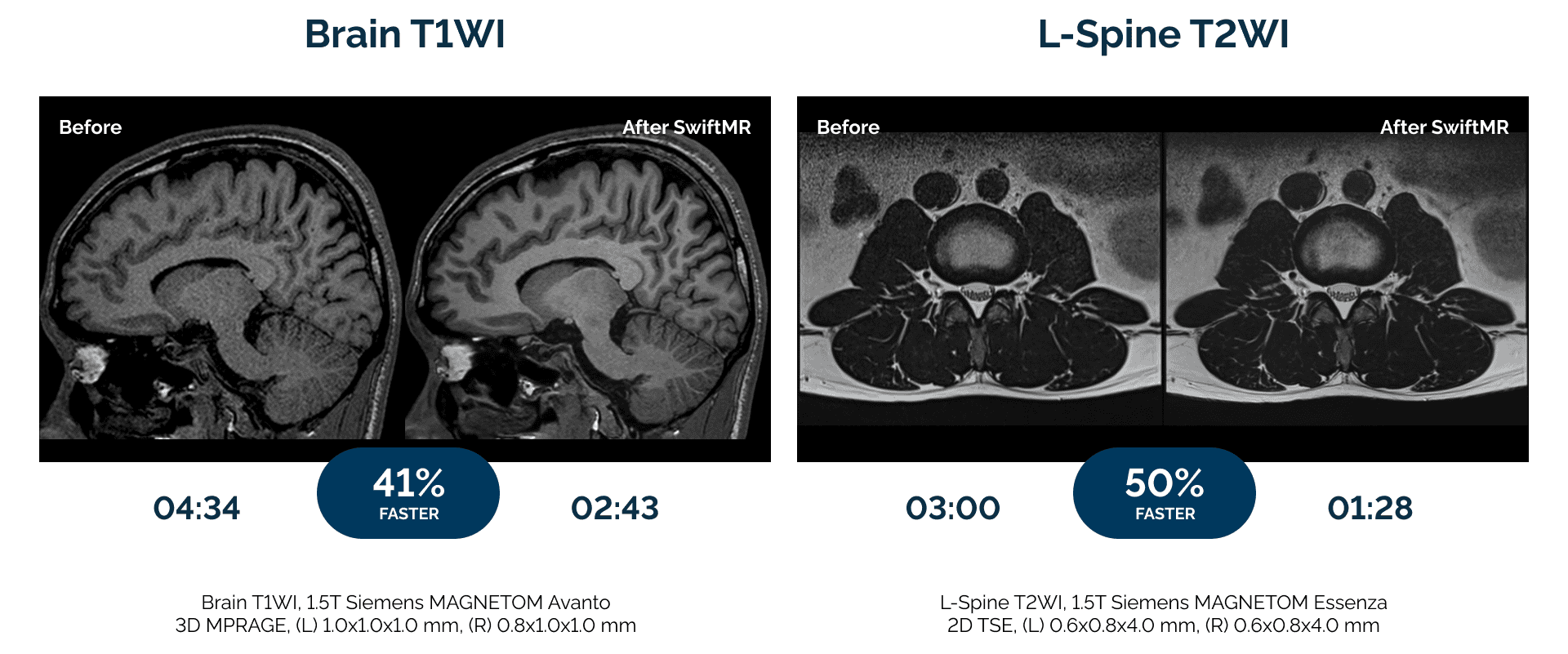
- Shorter scans – The shorter the scan, the easier it is for patients to stay still. Fujifilm’s ECHELON Synergy MRI features up to 50% scan time reduction over previous generation 1.5T MRI scanners, and a 70-cm-wide bore with a 62-cm-wide table to enhance comfort.
- Software tools – A study found that 15-20% of MRI scans require re-scan due to patient motion. ECHELON Synergy offers software that mitigates the impact of motion artifacts, making it easier and quicker to complete scans on fidgety patients.
- Open design – Put claustrophobic patients at ease and scanning needn’t stop mid-way through an exam. Providers are alleviating anxiety and boosting efficiency with Fujifilm’s OASIS Velocity MRI, which features a true open design, where patients have an unobstructed view for maximum comfort. OASIS Velocity also supports patients who weigh up to 660 pounds.
- Easy access – Improving comfort for all patient populations can help keep a facility competitive. Fujifilm’s APERTO Lucent is a powerful permanent magnet open-sided 0.4T MRI that delivers an optimal patient experience. Its unique single-pillar design provides ideal technologist-patient access, and the wide, laterally moving table lowers to 20 inches, ensuring easy access for pediatric, elderly, and/or injured patients.
Hospitals and imaging facilities across the U.S. rely on Fujifilm for state-of-the-art, patient-centric MRI systems. For example…
- Massac Memorial Hospital is addressing patient comfort by shortening scan times from 45 minutes to just 20 minutes.
- At Neurological Associates of Long Island “the big, wide gantry” makes a positive difference for patients undergoing brain and spine MRIs.
- West Feliciana Hospital is successfully addressing claustrophobia concerns with an open MRI.
Make patient comfort a top priority and give your MRI business a competitive edge with solutions from FUJIFILM Healthcare Americas Corp.