ECR 2026 opened yesterday with a light-filled opening ceremony that beautifully illustrated this year’s theme, “Rays of Knowledge.” The ceremony was conducted before an overflow audience in the Austria Center Vienna, with ECR 2026 President Prof. Minerva Becker proudly presiding over a mix of speeches, honorary awards, and musical performances for which ECR is famous.
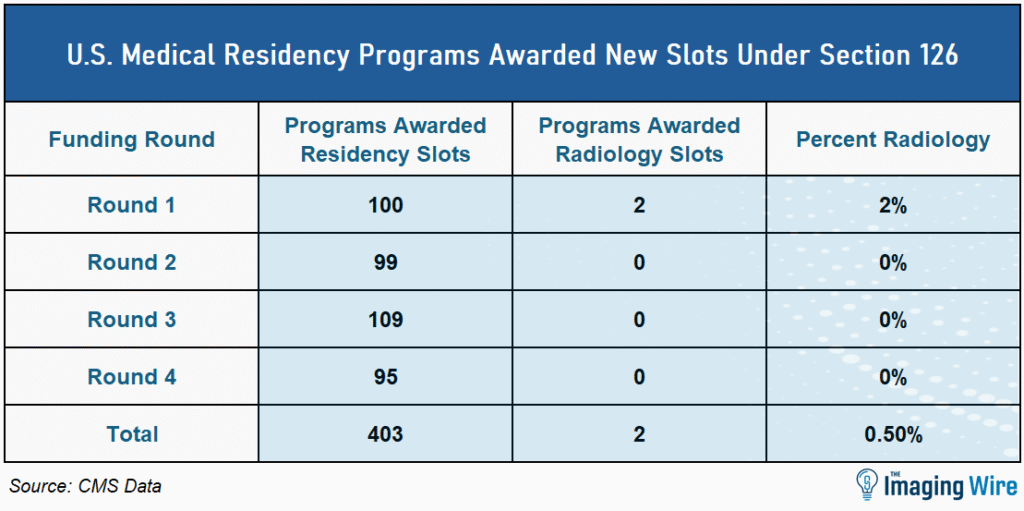
ECR 2026 is taking place as European radiology reaches an inflection point. The region has workforce shortages that are as serious (if not more so) than the U.S., and it must also accommodate rising demand for medical imaging.
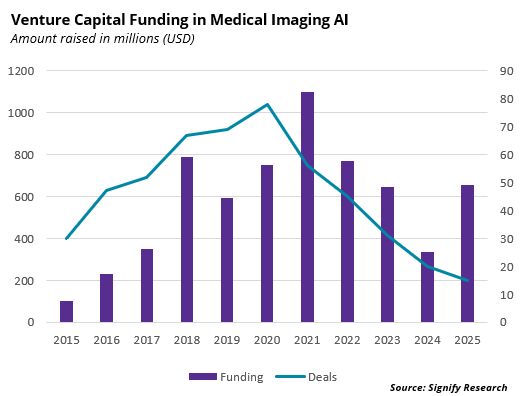
As in the U.S., artificial intelligence is being held up as a potential solution to enable radiologists to do more with less.
- In some ways, Europe is ahead of the U.S., having conducted large-scale prospective trials like MASAI to test AI’s value for tasks like breast screening. One country – Italy – has even recommended that AI be used routinely for breast screening.
But from a regulatory standpoint, skepticism toward AI may be even stronger in Europe than in the U.S.
- The European Union in 2024 implemented the AI Act to promote human-centered and trustworthy AI, and the act classifies AI algorithms as among the highest-risk devices. Some industry observers believe the act may already be slowing the introduction of new algorithms into the European market, even as the U.S. is removing regulatory guardrails on clinical AI.
Be that as it may, the ECR continues to reinforce its reputation as a forum for top-notch clinical content, and the first day of sessions did not disappoint. In particular, AI for lung cancer screening was a prominent focus, including the following sessions…
- Harrison.ai’s chest CT AI algorithm turned in 91% sensitivity for detecting pulmonary nodules in 1.1k LDCT scans, with an average of 1.12 false positives per case.
- Results from the RELIVE study of lung cancer screening in France showed that AI from Median Technologies boosted AUC for radiologists (0.843 vs. 0.828), with less experienced radiologists seeing a 4.8% AUC improvement.
- A survey of patients and clinicians in Northern Ireland found both groups were positive about using AI for lung cancer to reduce waiting times, but neither group liked the idea of autonomous AI.
- The LUNA25 challenge tested AI algorithms developed by five teams for estimating malignancy risk of lung nodules, finding that the top AI had standalone AUC performance better than the average of 75 radiologists (0.78 vs. 0.69).
- Dutch researchers tested four commercially available AI algorithms for LDCT lung screening, finding wide variation in sensitivity (77% to 92%).
- Carebot’s AI CXR software was used to analyze 96.5k chest X-rays from nine Czech hospitals over six months, finding 54 previously undiagnosed thoracic cancers.
The Takeaway
ECR 2026 continues through Sunday, and we’ll be on hand in Vienna to bring you the latest news from radiology’s premier pan-European conference. Stay tuned for our wrap-up newsletter next week, or follow along with our daily video reports on our LinkedIn and YouTube channels.