|
LVO Turf War | Breast MRI Cascade
April 17, 2022
|
|
|

|
|
Together with
|
|
|
|
“What I saw was expensive doctors, in expensive dark rooms, using software they hated.”
|
|
Us2.ai CEO, James Hare, on how a tour of a cardiology reading room inspired him to try to automate echocardiography.
|
|
|
|
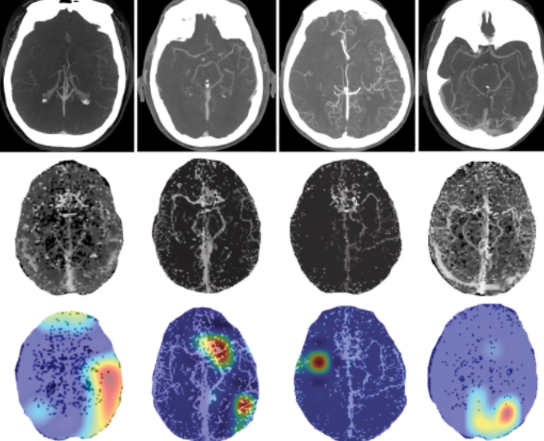
The FDA’s public “reminder” that studies analyzed by AI-based LVO detection tools (CADt) still require radiologist interpretation became one of hottest stories in radiology last week, and although many of us didn’t realize, it made a big statement about how AI-based coordination is changing the way care teams and radiologists work together.
The FDA decided to issue this clarification after finding that some providers were using LVO AI tools to guide their stroke treatment decisions and “might not be aware” that they need to base those decisions on radiologist interpretations. The agency reiterated that these tools are only intended to flag suspicious exams and support diagnostic prioritization, revealing plans to work with LVO AI vendors to make sure everyone understands radiologists’ role in these workflows.
This story was covered in all the major radiology publications and sparked a number of social media discussions with some interesting theories:
- One social post suggested that the FDA is preemptively taking a stand against autonomous AI
- Some posts and articles wondered if AI might be overly-influencing radiologists’ diagnoses
- The Imaging Wire didn’t even mention care coordination until a reader emailed with a clarification and we went back and edited our initial story
That reader had a point. It does seem like this is more of a care coordination issue than an AI diagnostics issue, considering that:
- These tools send notifications and images to interventionalist/surgeons before radiologists are able to read the same cases
- Two of the three leading LVO AI care coordination tools are marketed to everyone on the stroke team except radiologists (go check their sites)
- Before AI care coordination came along, it would have been hard to believe that stroke team members “might not be aware” that they needed to check radiologist interpretations before making care decisions
The Takeaway
LVO AI care coordination tools have been a huge commercial and clinical success, and care coordination platforms are quickly expanding to new use cases.
That seems like good news for emergency patients and care teams, but as the FDA reminded us last week, it also means that we’re going to need more safeguards to ensure that care decisions are based on radiologists’ diagnoses — even if the AI tool already informed care teams what the diagnosis might be.
|




|
|
Becoming Imaging AI Adopters
We talk a lot about radiology practices’ AI adoption, but usually don’t have much evidence to back it up. That changes with this new Arterys report detailing how and why 30 US radiology groups became imaging AI adopters.
|
|
COPC Ditches the Disk with Novarad
See how Novarad’s CryptoChart solution allowed Central Ohio Primary Care (COPC, 70 practices, 400 physicians) to make the transition to digital imaging sharing in this Healthcare IT News case study.
|
|
- Breast MRI Cascade: Breast MRI produces more diagnoses than mammography, but it also leads to far more follow-ups and patient costs. That’s from a new JAMA study of 9,208 women screened with breast MRI and 9,208 screened with mammography (w/ matched propensity scores), finding that the breast MRI cohort had far more follow-up imaging tests (18 vs. 13 per 100 women), procedures (22 vs. 5), physician visits (89 vs. 76), and new diagnoses (3.9 vs. 0.9) during the six months after their exams. That additional care also led to more overall ($869 vs. $305 per woman) and out-of-pocket ($573 vs. $542) breast-related costs.
- Remote Neurointerventions: MIT engineers developed a telerobotic neurointerventional platform that might allow neurovascular surgeons to remotely treat stroke or aneurysm patients at smaller/rural hospitals that typically lack on-site neurosurgeons. The remote surgeons would use a modified joystick and real-time fluoroscopy to control a robotic arm that performs the on-site procedure. Although this platform is in its early stages, remote neurosurgeons were able to remotely guide an interventional wire to a targeted location in a phantom after just an hour of training.
- AI Research Reckoning: A European Radiology review of 535 imaging AI academic studies (2015-2019) showed that even though many papers highlighted AI’s “expert-level results,” the studies were narrow in focus (mainly neuro and cancer) and lacking in methodological quality (only 2% prospective, just 14% externally validated). Noting the negative impact this has had on AI’s reputation and adoption, the authors urged AI researchers to diversify their clinical targets (more pathologies, modalities, use cases) and embrace best practices for AI training and study design. AI research methodology has surely improved since 2019, but the authors’ recommendations still seem relevant.
- Intermountain and SCL’s Model Merger: Intermountain Healthcare and SCL Health officially completed their merger, growing Intermountain into a $12B nonprofit health system with 33 hospitals and 385 clinics across seven Mountain West states. The merger will bring Intermountain deeper into Colorado, Montana, and Kansas, while advancing the former SCL Health sites’ digital transformation, and allowing them to tap into Intermountain’s patient value advantages.
- POCUS AR: Point-of-care vascular ultrasound company Dolphin Medical Imaging and augmented reality smart glasses company NuEyes announced a partnership to combine their respective products. When the NuEyes glasses and a Dolphin probe are connected via a Samsung smartphone or tablet, clinicians would be able to perform ultrasound-guided vascular access procedures without looking away from the patient. Dolphin appears to be more focused on smart glasses integration than most POCUS vendors, previously launching a partnership with mixed reality glasses company ThirdEye.
- Self-Scheduling Barriers: A new JACR study revealed that the use of online self-scheduling portals for mammography screening appointments is extremely low, and it’s even lower among traditionally disadvantaged patients. Analysis of 46k patients who received screening mammograms at an urban academic medical center in 2019 revealed that only 302 patients used the self-scheduling system (0.7%), and those patients were much more likely to be English speakers (OR: 21.3), White (OR: 1.7), have commercial coverage (OR: 1.5), and younger.
- Promaxo Adds Funding: Point-of-care MRI company Promaxo closed a $1.4M funding round (total now >$30M) that it will presumably use to support its product development and commercialization efforts. Leading with its small-size and low-cost, the Promaxo MRI is intended for use in physician offices and other clinical locations where MRI-based diagnostics and interventions traditionally haven’t been possible.
- Well Paid, Pretty Satisfied, and Largely Male: Medscape’s new Physician Compensation Report (n = 13k physicians, 29 specialties) showed that the average US radiologist earned $437k in 2021, representing a 5.6% increase from a COVID-impacted 2020. Radiology fell from the 6th to 8th top-earning specialty, but many radiologists still believed they were fairly compensated (63%, the 5th highest specialty), would pick the same specialty again (92%, 7th highest), and reported relatively low weekly paperwork labor (13.7hrs, 8th lowest). Radiology also remained one of the most male-dominated specialties (23% female, 7th lowest).
- Ultrasound for Bone Stress: A Journal of Ultrasound in Medicine study suggests that ultrasound might help sports medicine providers diagnose bone stress injury (BSI), when added to their standard clinical evaluation process. The study performed ultrasound and MRI exams on 37 athletes with suspected lower-extremity BSI (30 later confirmed), finding that ultrasound detected BSI with 0.80 sensitivity, 0.71 specificity, a 0.92 positive predictive value, and a 0.45 negative predictive value.
- Reinforcing Radiation Ethics: A new WHO policy brief called on healthcare providers to evolve their approach to ethical imaging, suggesting that its two foundational principles (procedure justification, optimized radiation protection) need reinforcements after 25+ years of rising imaging volumes. The WHO proposed new approaches focused on improving awareness (training, cultural changes) and formal efforts to create imaging ethics regulations and governance structures.
- CAD Voice Biomarker: Mayo Clinic researchers showed that a commercial voice biomarker can predict coronary artery disease events, suggesting that voice tests could eventually be used for CAD screening (and potentially affect CAD imaging use). The researchers had 108 patients referred for coronary angiography create three 30-second voice recordings, finding that patients with high baseline voice biomarkers had significantly higher risks of CAD events (hazard ratio: 2.61) and positive stress tests or coronary angiography results (hazard ratio: 3.13) during a 24-month median follow-up period.
|
|
Effortless & Efficient AI Adoption
Check out this GE Healthcare perspective on imaging AI’s adoption evolution, the AI ecosystem shift, and the importance of seamless AI integration.
|
|
- See Ochsner Lafayette General’s Director of Radiology, Emily Broussard, describe their “seamless” transition to Nuance PowerScribe One and how it has improved their reporting efficiency and quality.
- Us2.ai announced the global launch of its flagship echocardiography AI solution, leveraging a new $15M Series A round, and its unique abilities to completely automate echo reporting (complete editable/explainable reports in 2 minutes) and analyze every chamber of the heart (vs. just left ventricle with some vendors).
- See how Fujifilm Healthcare helped Arkansas Children’s Hospital imaging IT infrastructure evolve from departmental silos to an interoperable architecture that improved its radiology and IT teams’ day-to-day flexibility and future scalability.
- Variable heart rates and organ motion can make cardiac imaging a challenge for CT technologists. Discover how intelligent imaging guidance with Siemens Healthineers’ myExam Companion can help overcome these challenges, without compromising quality and consistency.
- Are you sure your imaging archive is safe and recoverable? See how Intelerad’s Cloud DR disaster recovery solution mitigates the many risks facing your archive by securely storing copies of every image.
- Explore how United Imaging is reinventing the medical imaging business, including downtime rebates, lifetime upgrades, and making sure their customers truly are successful.
- Canon Medical is making its way through the US on its 2022 Mobile Tour, bringing its products and solutions directly to hospitals and providers in 50 US cities. Tune in to see when Canon is coming to you and watch highlights from its tour stops along the way.
- After setting ambitious regulatory and commercialization goals, Lunit leveraged CARPL.ai’s platform and operational guidance to complete the clinical trials needed for its INSIGHT CXR and MMG AI tools’ FDA clearances.
- See how adopting ClearRead CT allowed Michigan’s Regional Medical Imaging’s radiologists to complete their chest CT reads faster and more accurately in this Riverain Technologies case study.
|
|
|
|
|