|
Interpreting AI | Diagnostic Declines
January 20, 2022
|
|
|

|
|
Together with
|

|
|
|
“We need algorithms that not only work, but explain themselves and show examples of what they’re basing their conclusions on. That way, whether a physician agrees with the outcome or not, the AI is helping to make better decisions.”
|
|
Duke Radiology professor, Joseph Lo PhD.
|
|
|
|
A team of Duke University radiologists and computer engineers unveiled a new mammography AI platform that could be an important step towards developing truly interpretable AI.
Explainable History – Healthcare leaders have been calling for explainable imaging AI for some time, but explainability efforts have been mainly limited to saliency / heat maps that show what part of an image influenced a model’s prediction (not how or why).
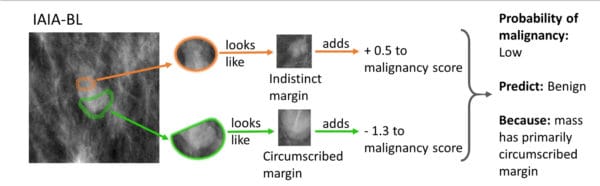
Duke’s Interpretable Model – Duke’s new AI platform analyzes mammography exams for potentially cancerous lesions to help physicians determine if a patient should receive a biopsy, while supporting its predictions with image and case-based explanations.
Training Interpretability – The Duke team trained their AI platform to locate and evaluate lesions following a process that human radiology educators and students would utilize:
- First, they trained the AI model to detect suspicious lesions and to ignore healthy tissues
- Then they had radiologists label the edges of the lesions
- Then they trained the model to compare those lesion edges with lesion edges from an archive of images with confirmed outcomes
Interpretable Predictions – This training process allowed the AI model to identify suspicious lesions, highlight the classification-relevant parts of the image, and explain its findings by referencing confirmed images.
Interpretable Results – Like many AI models, this early version could not identify cancerous lesions as accurately as human radiologists. However, it matched the performance of existing “black box” AI systems and the team was able to see why their AI model made its mistakes.
The Takeaway
It seems like concerns over AI performance are growing at about the same pace as actual AI adoption, making explainability / interpretability increasingly important. Duke’s interpretable AI platform might be in its early stages, but its use of previous cases to explain findings seems like a promising (and straightforward) way to achieve that goal, while improving diagnosis in the process.
|




|
|
COPC Ditches the Disk with Novarad
See how Novarad’s CryptoChart solution allowed Central Ohio Primary Care (COPC, 70 practices, 400 physicians) to make the transition to digital imaging sharing in this Healthcare IT News case study.
|
|
- DLIR Nodule Advantage: A new Radiology Journal study highlighted deep learning image reconstruction’s (DLIR) advantages for detecting lung nodules in ultra-low-dose chest CTs (ULD-CT). The researchers performed ULD-CTs on 203 participants with 1,066 nodules and reconstructed them using DLIR and iterative (ASIR-V) technologies. The DLIR-based images had higher nodule detection rates (75.8% vs. 73.3% w/ ASIR-V), less background image noise (23 HU vs. 29 HU), and produced nodule measurements that were closer to contrast-enhanced CT (long diameter difference from CECT: 6.2% vs. 9.2%; volume difference: 14.4% vs. 21%).
- INFINITT & Lunit Alliance: Enterprise imaging vendor INFINITT announced plans to distribute Lunit’s CXR and mammography AI solutions in North America, further expanding Lunit’s partner channel as it increases its focus on western markets. Although many PACS/AI partnerships seem to peak at the time of their press release, the two South Korea-based companies have been operating similar alliances in Asia for at least a year.
- Diagnostic Declines: Current Problems in Diagnostic Radiology lived up to its name, publishing a study that exposed massive diagnostic radiology reimbursement declines since 2011. Analysis of the 50 most common studies revealed a 44.4% Medicare reimbursement decline when factoring-in inflation, driven in part by big declines for several key modalities (MRI -60.6%, CT -44.4%, ultrasound -31.3%) and the fact that wRVUs and conversion factors didn’t keep up with inflation.
- Observe Acquires Biim Ultrasound: Observe Medical just expanded into the ultrasound segment with its acquisition of fellow Norwegian startup Biim Ultrasound for $21M. Biim Ultrasound is best known for its FDA-cleared Biim handheld that’s primarily used for needle and catheter guidance, and for its alliance with dialysis giant Fresenius Kidney Care (2,400 locations in the US). Observe plans to expand Biim Ultrasound throughout its European network and leverage Biim’s US presence to bring its other products stateside.
- DBT AI Pre-Screening: A new IBM-led study detailed a DBT AI system that could reduce radiologist workflows by 39.6% while improving breast cancer detection. The researchers trained, validated, and tested the model using 13,306 DBT exams from two health systems (tested w/ 5,182 DBTs, 459 cancers), finding that it eliminated cancer-free exams from reading worklists with similar sensitivity as radiologists (90.0% vs 90.8%) and with a far lower recall rate (6.9% vs. 9.2%). The AI model also beat five radiologists when reading 205 DBTs as a standalone system (0.84 vs 0.81 AUCs).
- RAYUS’ Utah Expansions: RAYUS Radiology opened two new imaging centers in Utah’s Wasatch region, expanding its presence in the state to nine locations and giving it 152 imaging centers nationwide. These Utah openings come just a few weeks after RAYUS added new centers in Minnesota and Maine, and follows a busy 2021 that included at least four territory-expanding acquisitions and the addition of 21 imaging centers.
- Japan Eases Up on AI: The Japanese government is reportedly planning to ease its healthcare AI regulatory requirements by reducing its initial AI review process, eliminating its process of reviewing every software update as if it were a new product, and potentially revising a rule that requires hands-on management of medical software. These moves are intended to drive the country’s AI adoption, noting that South Korea and the US have 2x and 6x more regulatory-approved healthcare AI products than Japan.
- Telerobotic Ultrasound Clinics: A University of Saskatchewan team demonstrated how telerobotic ultrasound might improve access to care in remote regions. The team created telerobotic ultrasound clinics in three indigenous communities using commercially-available technology, and performed 87 exams that were remotely-controlled by sonographers and read by remote radiologists. The radiologists rated 72% of the exams as sufficient for diagnosis, while 95% of the patients were willing to receive future telerobotic ultrasound exams (mainly due to reduced travel).
- Clarius’ Big Launch: Clarius Mobile Health just unveiled ten new handheld ultrasounds with some interesting tech and pricing/packaging updates. The Clarius HD3 scanners lead with their sleek form factor (30% smaller/lighter), Octal beamforming technology (faster frame rates & better resolution), and Clarius’ new mobile app (improves image quality, adds clinical packages). The launch also brings Clarius’ new “membership bundle” that provides a lower acquisition price ($2,995 vs. $4,900) and additional features (software, education modules, cloud storage) but adds a $595 annual subscription.
- Lung Cancer Screening Disparities: A new JACR study revealed some remarkable lung cancer screening adherence disparities. Analysis of an urban medical center’s 2015-2018 screening appointments (2,797 patients, 4,747 appointments) revealed that ~50% of patients did not return after their baseline exams and 41% missed at least one screening appointment. Patients who missed at least one exam were far more likely to identify as Black (1.5x more than White) and have Medicaid coverage (6.1x more than private, 4.6x than Medicare), while housing insecure patients had 5.3x higher odds of not returning after their baseline exam.
- Siemens’ iBreastExam Alliance: Siemens Healthineers will add UE LifeSciences’ iBreastExam handheld breast exam device to its U.S. portfolio, with the goal of improving routine breast exams among younger women with higher risk profiles (<40yrs, dense breasts and/or family history). The iBreastExam uses a panel of vibrating sensors to detect breast lumps at the point-of-care, without the radiation, discomfort, added appointments, or exam qualifications associated with mammography.
|
|
- This Bayer case study details how radiation benchmarking programs can help push CT dose exposure reduction initiatives from achieving compliance to driving quality.
- See how United Imaging’s new uCT ATLAS combines advancements in image quality, patient comfort, and operator efficiency to bring you one step closer to your masterpiece.
- Considering your short and long-term AI plan? Check out Canon Medical’s State of AI Roundtable, sharing insights into how imaging AI is being used, where it’s needed most, and how AI might assume a core role in medical imaging.
|
|
|
|
|