|
AMA Gets Quantitative | Lung Cancer Blood Test
January 13, 2022
|
|
|

|
|
Together with
|

|
|
|
“False: Radiologists who use AI will replace those who don’t.
True: Radiologists who understand AI will replace those who don’t.”
|
|
Raym Geis MD taking Curt Langlotz’s famous forecast one step further.
|
|

|
|
MD Anderson researchers developed a blood and risk-based test that could improve how we identify lung cancer screening candidates, potentially bringing more high-risk patients into screening while keeping more low-risk patients out.
The Blood + Risk Test – The test combines MD Anderson’s blood-based protein biomarker test with a lung cancer risk model that analyzes patient smoking history (the PLCOm2012 model). This combined test would be used to identify patients who should enroll in LD-CT screening programs.
The Study – MD Anderson researchers used the test to analyze 10k blood samples from 2,745 people with a +10 pack-year smoking history (including 1,299 samples from 552 people who developed cancer), finding that the blood + risk test:
- Identified 105 of the 119 people diagnosed with cancer within one year
- Beat the USPSTF 2021 criteria’s sensitivity (88.4% vs. 78.5%) and specificity (56.2% vs. 49.3%)
- Identified 9.2% more lung cancer cases than the USPSTF criteria
- Referred 13.7% fewer unnecessary screening patients than the USPSTF criteria
Blood-Based Momentum – Blood-based tests appear to be gaining momentum as a first-line cancer screening method, as the last 6 months brought a promising new MGH lung cancer test and a key validation milestone for the multi-cancer early detection blood test (MCED; detects 50 types of cancer).
The Takeaway – Although there’s still more research to be done, blood-based tests could bring more high-risk patients into LD-CT lung cancer screening programs, while reducing screening participation among patients who don’t actually need it. In other words, blood tests like these could address lung cancer screening’s two biggest challenges.
|




|
|
CVIS’ Cloud Advantages
This Diagnostic and Interventional Cardiology article details the unique advantages of cloud-based CVIS systems (off-property access, team collaboration), with insights from one Mississippi-based cardiologist on the benefits of Fujifilm Healthcare’s VidiStar CVIS.
|
|
|
|
The American Medical Association issued new CPT III codes for CT and MRCP quantification (see page 4), representing key milestones for quantitative and incidental/population health imaging.
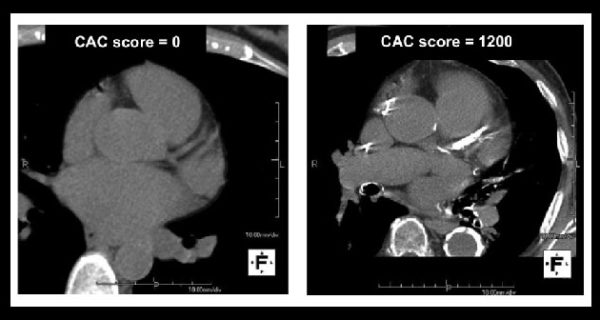
CT Quantification Codes – The AMA’s 2022 CPT III update includes two new codes for quantitative CT tissue characterization, interpretation, and reporting. These codes could be a big deal for AI firms and radiology departments hoping to launch CT-based population health solutions (and eventually bill for them), such as Nanox AI’s HealthCCSng CAC scoring product and UCSF’s automated CAC scoring system. They also come just six months after the AMA added a similar CPT III code for using AI to automatically detect vertebral fractures in existing CT scans (covering Nanox AI’s VCF solution).
MRCP Quantification Codes – The AMA also added CPT III codes for quantitative magnetic resonance cholangiopancreatography (QMRCP) interpretation and reporting. These codes are a solid step for MRCP quantification products like Perspectum’s MRCP+ and could help drive adoption for this far less-subjective MRCP interpretation method. In the process, it might even change ERCP’s role to a purely therapeutic procedure.
About CPT III Codes – Since there’s often confusion about CPT III codes, it’s worth noting that they are intended to help collect clinical data for emerging technologies / procedures to support future coverage and regulatory decisions. CPT III codes don’t have assigned RVUs, so actual reimbursements would be up to payors.
The Takeaway
It’s pretty clear that the AMA is starting to see value in image quantification, AI, and incidental detection. In the last six months the AMA has issued four quantitative imaging CPT III codes, all of which directly support key imaging AI use cases (CT tissue characterization, CT vertebral fracture detection, ultrasound tissue characterization, MRI post-processing) and two that support key population health and incidental detection applications (CT tissue characterization, CT vertebral fracture detection).
|




|
|
- One-in-Five False Positives: A new Cancer Journal study found that nearly one-in-five women in Norway received a false positive screening mammogram result over the course of 10 biennial screenings. Analysis of BreastScreen Norway data (n = 421k women, 50-69yr age, 1995-2019) revealed an 18% risk of receiving a false-positive result over 10 screenings / 20 years, and a 5% risk of receiving a false positive that led to an invasive procedure.
- Butterfly & URMC: Butterfly Network and University of Rochester Medical Center announced an alliance that will deploy Butterfly ultrasound systems across URMC (specifically to med students, PCPs, home care nurses), and lead to future handheld ultrasound research collaborations. Although Butterfly likely has other enterprise-wide health system partnerships, this is only the second we’ve seen, following a 2020 deal with Atrium Health.
- No CTs for Incidental COVID: A new Emergency Radiology study confirmed that CT isn’t effective for screening hospitalized patients for asymptomatic COVID. The Italy-based researchers performed chest CTs on 197 patients who were hospitalized for non-COVID reasons and had negative RT-PCR swab tests, finding that none of the 23 patients with suspicious CT scans actually had COVID. This might not surprise some readers, but it’s still notable given how many COVID-positive patients are currently hospitalized for other reasons.
- Another Aduhelm Setback: Biogen’s Aduhelm Alzheimer’s treatment experienced yet another setback after Medicare proposed only covering the controversial treatment for certain clinical trial patients. Aduhelm was originally expected to drive a wave of imaging exams (it requires brain PET for diagnosis & ongoing MRIs for monitoring), but the new drug has been surrounded by criticism about its effectiveness and costliness. In fact, a number of major health systems have already announced that they will not provide/prescribe Aduhelm (MGH, Cleveland Clinic, Mount Sinai, and the VA).
- LCS AI’s Drastic Workload Reduction: A new Lung Cancer journal study detailed an unsupervised AI system that could “drastically” reduce radiologists’ lung cancer screening workloads. The researchers had five blinded radiologists and Coreline Soft’s AVIEW LCS AI tool analyze 283 ultra low-dose CTs with at least one solid lung nodule, finding that the AI tool had a far higher false positive rate than the rads (18.7% vs. 2.1% to 8.8%), but a comparable false negative rate (2.8% vs. 1.4% to 12.4%) and negative predictive value (0.95 vs. 0.84 to 0.98). The authors estimate that using this tool for baseline reads could reduce rad workloads by between 77.4% and 86.7%.
- Healthcare Consumerism: The Economist published an article exploring how healthcare is quickly turning into a consumer product, making the case that new technologies are replacing care middlemen with more D2C models. Better data and an improving cloud infrastructure are given as examples of why we could be in the early stages of a transformation that’s likely to be “a negative prognosis for the hospital-industrial complex,” but a positive one for many patients. It’s unlikely that The Economist had radiology in mind, but radiology will definitely have to adapt to these changing patient behaviors and expectations.
- AI Education & Research: Imaging AI education and research seems to be becoming more common in radiology departments (at least depts with NIH funding), although there’s still plenty of room for these AI activities to expand. That’s from a new study in Current Problems in Diagnostic Radiology that surveyed 62 radiology departments that received NIH funding, finding that 29 (47%) departments offer AI education, 55 (89%) staffed at least one AI researcher, and 34 (55%) were affiliated with an AI research laboratory/center. However, most of these AI researchers and affiliated labs weren’t led by the radiology department and few departments had formal AI leadership roles.
- Canadian Backlogs: The Canadian Association of Radiologists is calling for more imaging equipment and staff to help overcome the country’s COVID-exacerbated imaging backlog. Canadians are currently waiting nearly three months for CT and MRI scans, and that doesn’t appear to be getting better, given that 75% of CAR members have not reduced their backlogs since the pandemic and 30% don’t expect wait times to return to pre-pandemic levels.
- Early Career, Late Day DBT Recalls: Patients are more likely to have their mammography screenings recalled if they undergo DBT exams and those exams are read by less-experienced radiologists later in their shifts. A new Radiology Journal study (n = 40k DBT exams, 57k DM exams, 18 rads) found that less-experienced radiologists’ DBT recall rates increased by 11.5% every hour of their shift, while their hourly DM recall rates remained relatively stable. Radiologists with more than five years of experience maintained stable hourly recall rates with both DBT and DM exams.
- DLIR CT Caveat: Deep learning image reconstruction (DLIR) technology might reduce CT dosage by 65% and improve perceived image quality, but the technology might not be appropriate for assessing smaller liver lesions. A new Radiology Journal study had three radiologists assess standard dose and DLIR-enhanced CTs from 51 patients with colorectal cancer and liver metastases (161 liver lesions, 0.7cm mean size). The radiologists found the DLIR images to have higher image quality and signal-to-noise ratios, but they detected far more ≤0.5cm lesions with the standard dose CTs (63 vs. 47 out of 65).
|
|
- Check out this Imaging Wire Show featuring GE Healthcare’s US & Canada MRI leader, Brian Murphy, discussing MRI’s evolution and how AIR Recon DL is eliminating MRI’s signal, speed, and resolution compromise.
- United Imaging’s uCT ATLAS ultra-premium CT scanner delivers imaging that covers it all. That means 16 cm whole organ coverage, enabling a non-contrast brain in a half-second with a single rotation. That also means whole-heart coverage combined with 0.25 second rotation speed, providing high-quality and low-dose images within one heartbeat.
- CD burning issues? Check out this one-minute video showing how Novarad’s CryptoChart image sharing solution allows patients to easily access and share their medical images using personalized, highly secure QR codes (not CDs).
|
|
|
|
|